Did you know that Ankylosing Spondylitis typically begins in early adulthood, usually between the ages of 17 and 45. However, it can develop at any age, and there have been cases of onset in childhood or later in life.
AS tends to affect men more frequently than women. The male-to-female ratio of AS patients is often reported to be around 2:1 or 3:1. However, it’s important to note that AS can and does affect both genders.
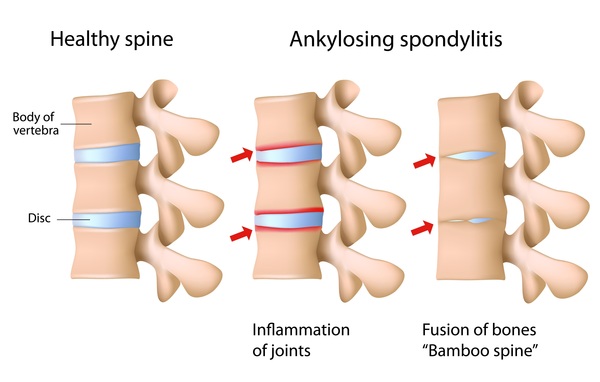
Ankylosing Spondylitis (AS) is chronic inflammatory autoimmune disorder primarily affecting the spine and sacroiliac joints. This condition can lead to severe pain, stiffness, and even fusion of the spine, significantly impacting the quality of life for those affected. While modern medicine offers treatments like non-steroidal anti-inflammatory drugs (NSAIDs) and biologics to manage symptoms, Ayurveda provides a holistic approach to the management of AS. In this article, we will explore the principles of Ayurveda and how it can be employed to manage ankylosing spondylitis.
Causes of Ankylosing spondylitis
The cause of ankylosing spondylitis remains unknown to researchers, but there is evidence suggesting that a combination of genetic and environmental factors may contribute to its development. One known genetic factor associated with an increased risk of ankylosing spondylitis is the HLA-B27 gene. It’s important to note, however, that having this gene doesn’t guarantee you will develop the disease, as many individuals with the gene never do. This underscores the significance of environmental factors in the disease’s development.
While researchers have identified several gene variations that might be linked to ankylosing spondylitis, HLA-B27 is currently the primary known gene associated with an elevated risk of developing the condition.
Who gets Ankylosing spondylitis
Ankylosing spondylitis can affect individuals of any background, but there are specific factors that may heighten your susceptibility to the condition. These factors encompass:
- Family History and Genetics: If you have a family history of ankylosing spondylitis, your risk of developing the disease is elevated.
- Age: While most individuals start experiencing ankylosing spondylitis symptoms before the age of 45, it’s worth noting that some may develop the condition during childhood or adolescence.
- Other Underlying Conditions: Individuals who have other autoimmune conditions like Crohn’s disease, ulcerative colitis, or psoriasis may be at a higher risk of developing ankylosing spondylitis.
Symptoms of Ankylosing Spondylitis
Ankylosing Spondylitis (AS) can manifest in various ways, and its symptoms can vary from person to person. Here are the common signs and manifestations:
- Lower Back and Hip Pain: The hallmark symptom of AS is lower back and hip pain, often accompanied by stiffness. This discomfort tends to worsen during periods of inactivity or rest, leading to increased pain during the night or after prolonged sitting. Fortunately, movement and exercise can help alleviate this pain.
- Progressive Symptoms: Over time, AS symptoms may extend to affect other regions of the spine and body. The condition can lead to chronic pain in some individuals, while others may experience intermittent episodes of mild pain. Symptoms often worsen during “flares” and improve during periods of remission.
- Joint Involvement: AS can extend beyond the spine, causing pain, stiffness, and inflammation in other joints like the ribs, shoulders, knees, or feet.
- Breathing Difficulties: When the joints connecting the ribs are affected, individuals with AS may experience difficulty taking deep breaths, leading to breathing issues.
- Eye Complications: Uveitis, an inflammation of the eye, can cause vision changes and eye pain in AS patients.
- Fatigue: AS can be physically exhausting, leading to persistent fatigue and a constant feeling of tiredness.
- Loss of Appetite and Weight Loss: AS may reduce appetite and result in weight loss, which can be particularly concerning in severe cases.
- Skin Issues: Some AS patients may develop skin rashes, especially those with psoriasis.
- Abdominal Discomfort: Abdominal pain and loose bowel movements may occur, although these symptoms can be less common than others.
It’s essential to remember that AS symptoms are highly variable, and individuals may experience a combination of these symptoms to varying degrees. Early diagnosis and appropriate management can help improve the quality of life for individuals with Ankylosing Spondylitis.
Stages of Ankylosing Spondylosis
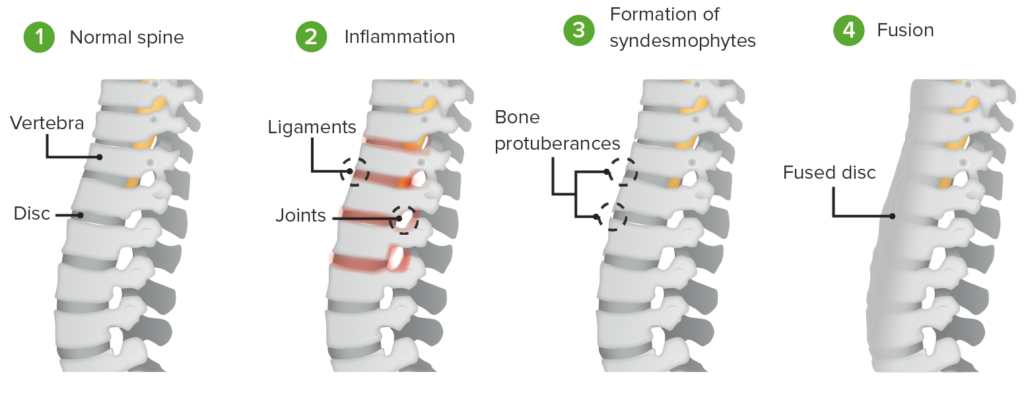
Ankylosing spondylitis (AS) is a progressive condition that primarily affects the spine and sacroiliac joints. The progression of AS can vary from person to person, but it typically occurs in several stages, each with its own characteristics and challenges. It’s important to note that not everyone with AS will experience all of these stages, and the severity and timeline can differ. Here are the general stages of ankylosing spondylitis:
- Early Stage (Inflammatory Stage):
- Inflammatory Pain: This is the initial stage of AS, marked by recurrent, inflammatory lower back pain and stiffness. The pain tends to be worse in the morning and after periods of inactivity.
- Fatigue: Many individuals experience fatigue as a common symptom during this stage.
- Gradual Progression: The inflammation gradually spreads and affects the sacroiliac joints, leading to pain and stiffness in the lower back and buttocks.
- Intermediate Stage (Adaptive Stage):
- Fusion Begins: As AS progresses, the inflammation can lead to the formation of new bone in the spine, a process known as ossification. This can result in the fusion of spinal vertebrae.
- Reduced Mobility: The fusion of the spine can cause a reduction in spinal mobility and flexibility. The individual may start to experience difficulty in bending, twisting, or turning.
- Late Stage (Advanced Stage):
- Severe Spinal Fusion: In the advanced stage, spinal fusion becomes more extensive, and the spine may lose its natural curvature.
- Decreased Lung Expansion: Spinal fusion can affect the chest wall’s flexibility, leading to decreased lung expansion and potentially causing breathing difficulties.
- Complications and Extra-Articular Involvement:
- Joint and Soft Tissue Involvement: AS can affect other joints besides the spine, such as the hips, shoulders, knees, and ankles. In some cases, it may also involve the tendons, ligaments, and other soft tissues.
- Eye Inflammation: Uveitis, inflammation of the eye, can be a recurring issue in some individuals with AS.
- Cardiovascular Complications: AS is associated with an increased risk of cardiovascular problems, including aortic valve issues.
It’s important to emphasize that not everyone with AS progresses through all these stages, and the rate of progression varies. Early diagnosis and appropriate management, including medication, physical therapy, and lifestyle modifications, can help slow down the progression of AS, manage symptoms, and improve the individual’s quality of life. Regular monitoring and follow-up with a healthcare professional who specializes in rheumatology are crucial for effectively managing this condition.
The treatment for Ankylosing Spondylitis (AS) in allopathic medicine
The treatment for Ankylosing Spondylitis (AS) in allopathic medicine focuses on managing the symptoms, reducing inflammation, and improving the patient’s quality of life. While there is no cure for AS, a combination of medications, physical therapy, and lifestyle modifications can help control the condition. Here are some common treatments used in allopathic medicine for Ankylosing Spondylitis:
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs, such as ibuprofen and naproxen, are often the first line of treatment for AS. They help reduce pain, inflammation, and stiffness. However, long-term use should be monitored, as NSAIDs can have side effects on the gastrointestinal system and kidneys.
- Disease-Modifying Antirheumatic Drugs (DMARDs): In cases where NSAIDs alone are not effective, DMARDs like sulfasalazine may be prescribed to reduce inflammation and slow the progression of AS. Methotrexate is another DMARD sometimes used in refractory cases.
- Biologic Drugs: Biologic medications, such as tumor necrosis factor-alpha (TNF-alpha) inhibitors like etanercept, adalimumab, and infliximab, are often prescribed for moderate to severe AS. They target specific immune system proteins responsible for inflammation and can be highly effective in managing symptoms.
- Corticosteroids: In some situations, corticosteroids like prednisone may be used for short-term relief of severe inflammation and pain. However, these drugs are generally not recommended for long-term use due to their potential side effects.
- Physical Therapy: Physical therapy plays a crucial role in the management of AS. Physical therapists can provide exercises and techniques to improve flexibility, strength, and posture, helping patients maintain mobility and reduce pain.
- Lifestyle Modifications: Lifestyle changes can have a significant impact on AS management. This includes maintaining a good posture, regular exercise, and avoiding smoking, as smoking can worsen the condition.
- Surgery: In severe cases where AS has led to significant spinal deformity or disability, surgical interventions may be considered. These surgeries can include spinal fusion or joint replacement procedures.
- Pain Management: Pain management techniques, such as nerve blocks or radiofrequency ablation, may be used to alleviate severe pain in specific joints.
Ayurvedic Approach to Ankylosing Spondylitis
In Ayurveda, each individual is unique, and treatment is personalized based on one’s constitution or dosha (Vata, Pitta, and Kapha) and the imbalance present. Ankylosing Spondylitis, in Ayurvedic terms, is often attributed to an imbalance of Vata and Pitta doshas, with an emphasis on the involvement of Ama (toxins) in the joints and tissues.
- Dietary Modifications:
Ayurveda places significant emphasis on diet in the management of AS. A balanced and individualized diet can help reduce inflammation and promote healing. Here are some dietary recommendations for AS:
- Anti-inflammatory Foods: Incorporate foods with anti-inflammatory properties, such as turmeric, ginger, garlic, and green leafy vegetables, into your daily meals.
- Avoid Trigger Foods: Eliminate or reduce foods that can aggravate inflammation, such as dairy, red meat, processed foods, and alcohol.
- Digestive Health: Enhance digestive fire (Agni) with spices like cumin, coriander, and fennel. Proper digestion helps prevent the accumulation of Ama, which can worsen AS.
- Herbal Remedies:
Ayurveda offers a wide range of herbal remedies to manage AS. Some commonly used herbs include:
- Ashwagandha (Withania somnifera): Known for its anti-inflammatory and analgesic properties, ashwagandha can help reduce pain and inflammation in AS.
- Turmeric (Curcuma longa): Curcumin, the active compound in turmeric, is a potent anti-inflammatory agent that can provide relief from AS symptoms.
- Guggul (Commiphora mukul): Guggul resin has demonstrated anti-inflammatory properties and can be beneficial in managing joint pain.
- Panchakarma:
Panchakarma is a set of therapeutic procedures in Ayurveda that aim to detoxify and rejuvenate the body. It can be highly effective in managing AS by eliminating Ama and balancing the doshas. Panchakarma therapies may include:
- Virechana (Purgation): Administering herbal laxatives to remove toxins from the body.
- Basti (Enema Therapy): Using herbal decoctions or oils to cleanse and nourish the colon.
- Swedana (Sweating): Inducing sweating through steam or herbal therapies to eliminate toxins.
- Yoga and Exercise:
Regular exercise is crucial for managing AS, as it helps maintain flexibility and prevent the fusion of the spine. Yoga, in particular, offers gentle stretches and postures that can improve mobility and reduce pain. Consult with an experienced yoga instructor who can tailor a routine to your specific needs. - Lifestyle Modifications:
Ayurveda advocates for a balanced lifestyle to maintain overall health. Stress management techniques such as meditation and deep breathing exercises can be beneficial for AS patients. It’s also essential to ensure an adequate amount of rest and sleep to support the body’s healing processes. - Ayurvedic Medicines:
In Ayurveda, there are specific formulations that are used for rejuvenation and strengthening of the body. These can be prescribed by an Ayurvedic doctor based on the individual’s constitution and the nature of the AS imbalance.
Please remember that Ankylosing Spondylitis is a serious condition and requires medical intervention. The above-mentioned remedies including herbal remedies or lifestyle modifications are not treatment in itself, but may become part of the treatment prescribed by a qualified Ayurveda doctor.
Can Ayurveda cure Ankylosing Spondylitis completely
Ankylosing Spondylitis is a progressive autoimmune condition and it cannot be cured through any form of treatment. Is a challenging condition that can significantly impact a person’s life. While modern medicine provides effective pharmacological treatments, Ayurveda offers a holistic approach that focuses on addressing the root cause of the condition and promoting overall health and well-being.
Why is Ayurveda considered better for managing Ankylosing Spondylitis?
Ankylosing Spondylitis treatments are long term since it is a progressive autoimmune condition and it cannot be cured through any form of treatment.

Ayurveda treatments mainly focus on stabilizing the disease progress and bringing down the symptoms. Ayurveda treatments have a disease modifying action where the inflammatory damages that happened due to ankylosing can be reduced and long-term stability can be achieved.
Because Ankylosing Spondylitis necessitates extended treatment, a holistic approach involving an initial combination of Ayurvedic oral medication, then external medical applications, and lifestyle modifications offers a natural means to manage the condition effectively, without the need for long-term prescription drugs or the risk of side effects.”
At UWAY our team of doctors have been successfully treating and managing various stages of Ankylosing Spondylosis with great success. The success can be attributed to sticking to the core Kerala Ayurveda medical protocols and using modern diagnostics wherever necessary.


